Dental professionals and their teams hold a key advantage in identifying sleep apnea and craniofacial pain. This is largely due to their comprehensive training in assessing the overall health of patients. Regular dental visits, typically twice a year, enable dentists to notice specific traits, characteristics, and habits that could indicate a susceptibility to a range of systemic conditions. It’s now crucial to integrate screenings for sleep apnea and craniofacial pain into dental practices.
Currently, obstructive sleep apnea (OSA) affects approximately 1 billion individuals aged 30 to 69 worldwide. The incidence of OSA is on an upward trend globally, exacerbated by rising obesity levels, a primary contributor to the condition.
Furthermore, about 10% of the adult population experiences craniofacial pain, with women being twice as likely to suffer from this condition compared to men. This type of pain ranks as one of the leading causes of chronic discomfort, trailing only behind back, neck, and knee pain. While acute craniofacial pain often stems from dental issues, chronic cases are usually linked to musculoskeletal problems, including temporomandibular joint disorders (TMDs).
The widespread impact of OSA and craniofacial pain on people around the world underscores the urgent need for effective treatment options. Dentists are strategically positioned to meet this need due to their regular interaction with patients and the nature of their work.
To rise to this challenge, it is imperative for dental professionals to deepen their understanding of dental sleep medicine and the management of craniofacial pain. This enhanced knowledge is essential for providing the highest level of care to those affected by these conditions.
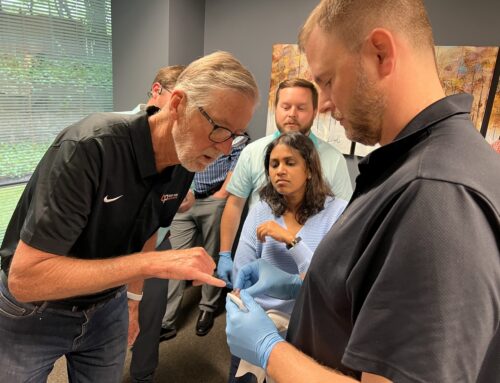
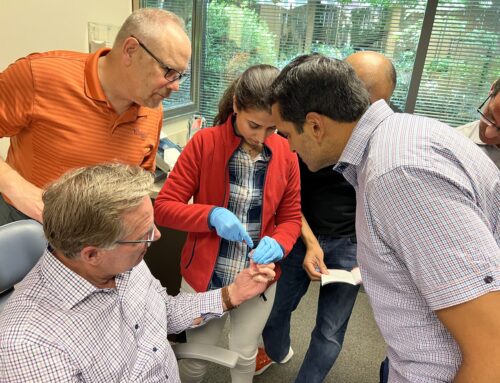
With that, join us for a four-part residency on craniofacial pain and dental sleep medicine at Tufts University School of Dental Medicine.
Course topics we will cover
Throughout the four parts of this residency, there are a variety of topics we will cover about craniofacial pain and dental sleep medicine.
For craniofacial pain, we will cover:
- Anatomy Related to Sleep and TMD
- Neuroanatomy related to pain
- TMJ Disorder
- Muscle Disorders
- History taking for pain
- Imaging for TMD and Sleep
- Pharmacology for Pain
- Injections
- Basic Concept of Pain
- TMJ Splint Therapy
- Neurovascular/Neuropathic Pain
- Understanding Oral Appliance Therapy for Pain and Sleep
When it comes to dental sleep medicine, the topics we will cover are:
- Physiology of Normal and Abnormal Sleep
- Classification of Sleep Disorders and HST/PSG
- Screening for Dental Sleep Medicine and Identifying Patients within your Practice
- Treatment Options for OSA
- Oral Appliance Selection and Procedures
- Dental Sleep Medicine Case Management
- Building a TMD and DSM Practice
- Pediatric Sleep Medicine
- Getting paid – medical billing
Take the next step in advancing your education and dental practice by signing up today! We look forward to seeing you in the residency and helping you learn more about craniofacial pain and dental sleep medicine.