Improve your knowledge of craniofacial pain and dental sleep medicine
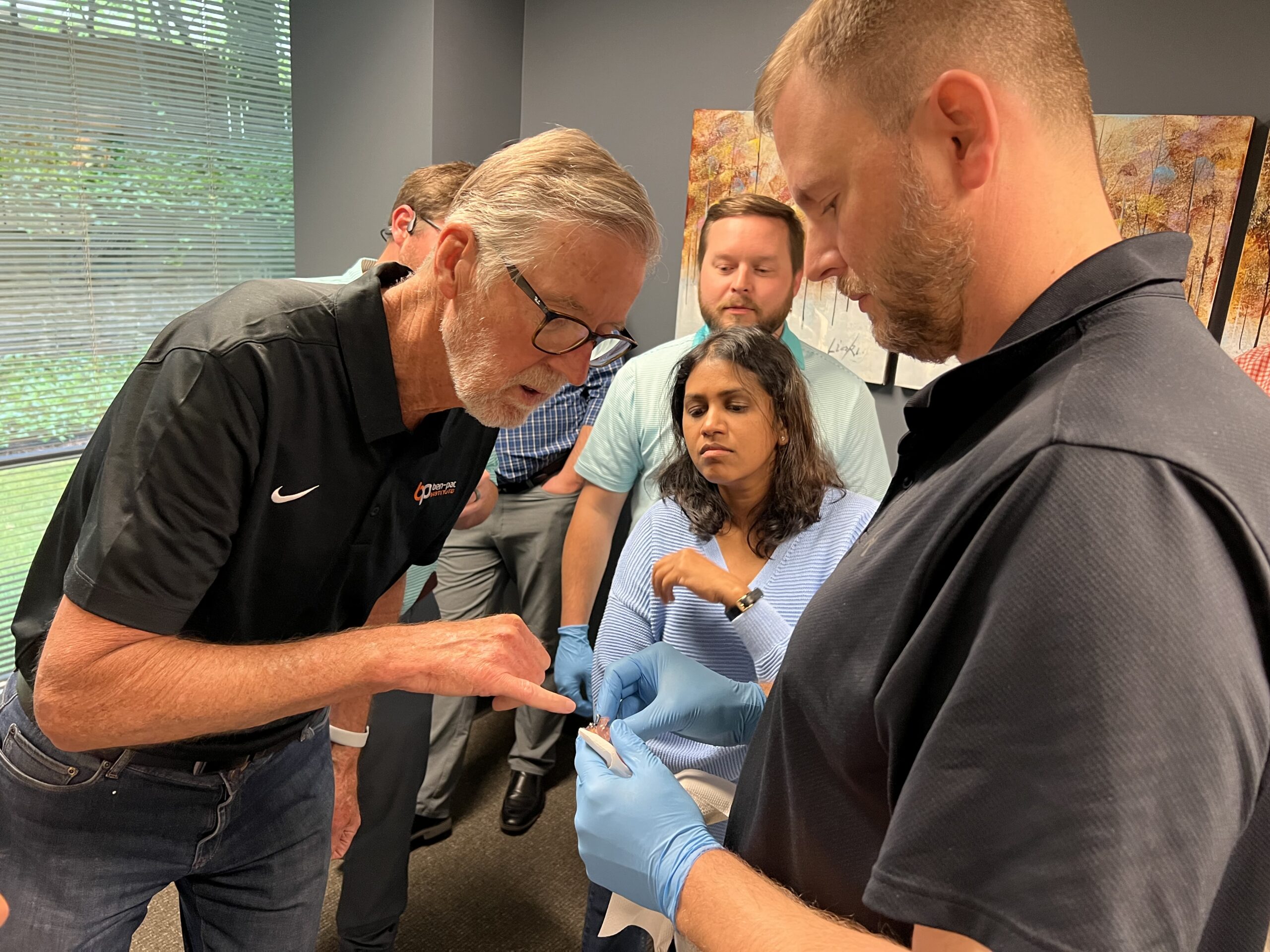
Embarking on a journey through the realms of craniofacial pain and dental sleep medicine offers an invigorating frontier for dental professionals eager to deepen their expertise and enhance their [...]